A (micro)bioscience roadmap to urban ‘ecosystem health’
By Jake Robinson
In general, our urban environments are not very healthy places—for us or the rest of nature. As microbial communities are foundational to a healthy ecosystem, we must start restoring and designing our urban environments with microbes in mind. This is what the Microbiome-Inspired Green Infrastructure or ‘MIGI’ concept is all about.
MIGI can be divided into two conceptual arms. The first is human health, i.e., through the microbiome lens, how can we restore and design urban environments to enhance human health and wellbeing? The second is ecosystem functionality and resilience, i.e., through the microbiome lens, how can we restore and design urban environments to enhance ‘ecosystem health’?
In terms of human health, there are three critical questions to ask in this research field:
1. Does exposure to ‘natural environments’ change the human microbiome?
2. Does exposure to environmental (micro)biodiversity affect human health?
3. Do urbanisation, habitat design and restoration affect microbial exposure routes and potential?
Right then, what do we know about question 1?
Several studies now demonstrate that exposure to urban green spaces can indeed change the human microbiome. In 2020, Australian microbiome scientist Dr Caitlin Selway and team revealed that spending a relatively short period (roughly an hour) in an urban park altered the microbiome of the human skin and respiratory lining. They observed a significant post-exposure increase in the number of bacterial species (alpha diversity) on the skin and nasal lining. Moreover, the community composition (beta diversity) was significantly different after green space exposure. The bacterial communities on the skin became very similar to those found in the soil and on plant leaves.
Another cool experiment by the Adelaideans was a study led by soil scientist Dr Craig Liddicoat in 2020. They found that exposing germ-free mice to trace levels of soil dust from biodiverse environments significantly altered the gut microbiome of the mice. Not only this but the presence of a soil-dwelling bacterium called Kineothrix alysoides found in the guts of the mice associated with a significant reduction in anxiety-like behaviours.
Jumping over to continental Europe and we find that Finnish research groups are bustling in this space too. In 2020, microbiome scientist Dr Marja Roslund led a study that assessed the effects of transforming desolate schoolyards into biodiverse spaces by bringing in local forest materials (soil, shrubs, grass etc.). They also studied several schoolyards without natural features. These latter sites acted as an experimental control. Remarkably, they found that after 28 days, the diversity of the microbiomes of the children who played in the biodiverse yards had significantly increased with enhancements in their immune systems. They followed this up a year later and found similar results with significantly fewer pathogenic bacteria in the schoolyards with the biodiversity intervention.
A final example, also by the Finnish microbiome scientists, involves sandcastles! A study led by Dr Nan Hui in 2019 revealed that inoculating children’s sandpits with soil and plant material changed the skin microbiome of the kids; the diversity of bacteria increased, and the number of pathogenic bacteria decreased.
In summary, mounting evidence supports the idea that spending time engaging with biodiversity can indeed change the human microbiome. There’s an important—Marja Roslund’s (and team) study is the only one to study long-term impacts. Therefore, investigating the longitudinal effects of engaging with green and blue spaces on the human microbiome needs to be one of the main priorities for researchers in this field. Further, we also need more research assessing the quality of the green space (i.e., the composition and structure) and its impact on the human microbiome.
What do we know about question 2?
So, we have evidence to support the (perhaps intuitive!) idea that spending time in ‘nature’ can change the microbiome, but does it affect human health via the microbiome?
Well, we have the evidence above from Marja’s studies showing enhanced immunity following the biodiversity intervention and the previous studies showing that engaging with biodiversity can potentially reduce the relative abundance of pathogens on the body. But we also have population-level studies to provide support. For example, there are two geocultural populations in the USA—the Amish and the Hutterites—who are very similar regarding their genetics and geography. However, one thing that differs between these populations is their farming practices. The Amish still use relatively traditional farming methods—they’re regularly ‘hands-on’ with the soil, the plants and the animals. Whereas the Hutterites have moved towards more modern and mechanised farming practices and are therefore less exposed to the (micro)biodiversity of the land.
Importantly, researchers found that inflammatory diseases (such as asthma) were significantly more prevalent in the Hutterites. They went a step further and investigated the microbiomes of the house dust of these two populations and found significant differences. They also inoculated the house dust microbiota into mice and found that the Amish microbiota was more protective of asthma. Another small study has since inoculated the microbiota from the faeces of these populations into mice and had similar results—the Amish microbiota was more protective of inflammatory conditions. This is corroborated by many studies linking the traditional farm environment to reduced allergic diseases.
Interestingly, similar trends have been shown in similar populations in Finland and Russia—again linking disparate health outcomes to changes in lifestyles and surrounding (micro)biodiversity. These studies support the Old Friends hypothesis or the Biodiversity hypothesis, which posit that reduced exposure to diverse environmental microbes due to biodiversity loss and sociocultural barriers has led to an explosion in immune disorders. Another recent study that supports these hypotheses is one by Dr Geoffrey Donovan and team in 2021. They found that children who lived in areas with less biodiversity were 35% more likely to get childhood acute lymphoblastic leukaemia.
The final question was: do urbanisation, habitat design, and restoration affect microbial exposure routes and potential?
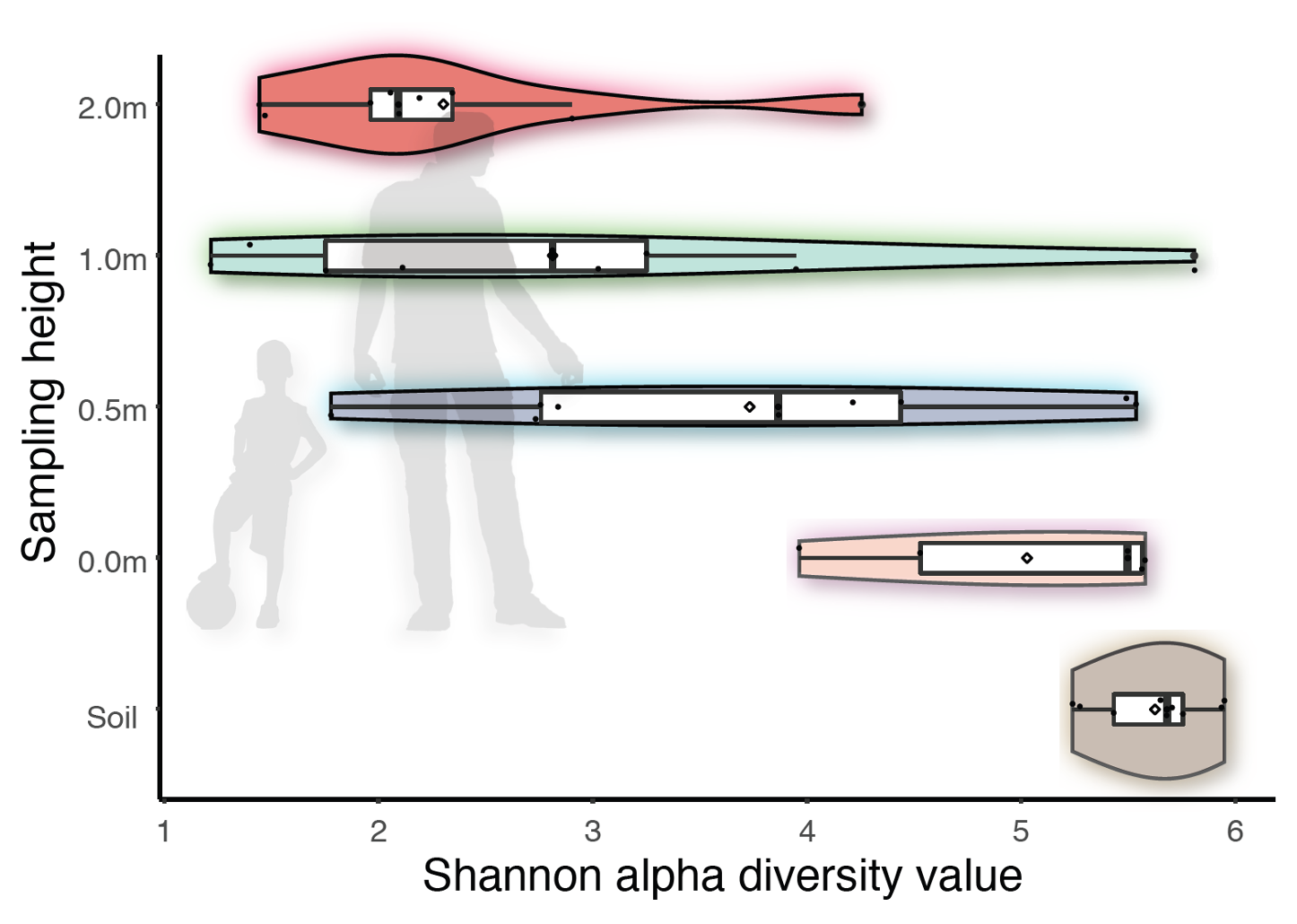
To explore this, I can talk about several studies I’ve been involved in. Firstly, we’ve demonstrated that vertical stratification occurs from the ground and up to 2 meters in the air column. This means that the alpha diversity (species richness/evenness) of bacteria decreases the further away you get from the soil.
We also found that vegetation complexity (as shown by others such as Dr Gwynne Mhuireach) influences the microbial makeup of the air. In areas with more trees and diverse vegetation, the alpha diversity of microbes in the air is higher.
This is thought to be important due to diverse microbes providing critical roles in immunity and potentially other functions in our bodies. Further, our studies have provided initial evidence that greater vegetation complexity may also reduce the abundance of pathogens in the air. This is supported by other studies, such as one by Dr Li and team in 2021, who showed the relative abundance of pathogens in the air and soil decreased with increasing tree abundance. We also know that microbial diversity is higher downwind from a source of biodiverse vegetation and that pollution interacts with the microbiome, with potentially significant implications for our health.
Therefore, from a human and environmental microbiome perspective, there is growing evidence to demonstrate:
Different exposure routes (and 3-dimensional space/structure matters)
Transfer of microbes from the environment to humans
Associations between (micro)biodiversity exposure and human health
How behaviour, urbanisation, and design/restoration affect these phenomena
Considering all this information (plus a whole host of other studies not mentioned here), I think we can start—via the microbiome lens—to restore and design our urban environments with human health in mind.
In practice
Here are some updates on how we’re working on translating the research into practice:
· My colleagues and I have published an overlay to the Royal Institute of British Architects ‘plan of works’ to show how microbiomes can be considered at each stage of an urban development project.
· We also have a MIGI review article accepted in the Architectural Research Quarterly journal (soon to be published).
· We’ve applied for funding to work collaboratively with practitioners to help address conceptual and operational barriers.
· We continue to do on-the-ground and in-the-lab research to help fill in the gaps.
· We’ve been working with large urban developers. One project involved creating a Design Guide tool that developers can use to assess the condition of their sites (via a risk assessment-style process) and understand how they can design/change the site with considerations for the environmental microbiome and human health.
The above assessment is based on a set of six parameters:
1. Features that promote compositional and functional diversity of the microbiome (e.g., vegetation diversity/structure, vertical stratification, soil type/quality, habitat connectivity, microbial inoculations)
2. Features that reduce the likelihood of a high relative abundance of pathogens (e.g., monocultures, disturbed habitats, synthetic chemicals, and pollution likely increase them)
3. Features that promote direct human engagement with diverse microbiomes (e.g., accessibility, community engagement activities, foraging)
4. Features that increase the wildlife value of the site (habitat quality, composition/structure, connectivity, sensitive lighting schemes)
5. Bio-integrated architecture (e.g., suitable conditions for cryptogams (lichens, mosses, ferns etc.), green roofs/walls)
6. Features that promote long-term ecological resilience (e.g., legacy planning, management strategies, organisational culture)
I will save the second conceptual arm of MIGI (ecosystem functionality and resilience) for another blog post as this is already mahoosive! But in summary, I think that yes, we can restore and design urban ecosystems—with explicit considerations for the microbiome—to enhance human health and ecosystem functionality.
All of this must form part of a holistic, ecological and life-long approach to ‘health creation’—for ourselves and the rest of nature.
Find out more in my forthcoming book Invisible Friends—soon to be published by Pelagic Publishing